608
CREDITS: Wikipedia
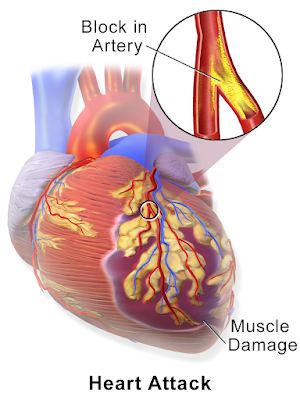
A heart attack or stroke can catch people off guard, even if they believe they are not at risk. Now, a new model developed by UConn Health researchers might help us detect cardiac disease better.
Heart attacks and strokes are the leading causes of mortality in the United States, with cholesterol plaques obstructing blood arteries accounting for 70% of all deaths. Despite the high incidence of cardiovascular illness, our best efforts to forecast who is at risk of catastrophic events such as a stroke or heart attack have been unsuccessful.
Body mass, waist circumference, and the percentage of different fats in a person’s blood are all factors in current risk models. However, using that model to correctly forecast whether someone would have a heart attack in the next five years, for example, is difficult. Other elements, according to many academics, must be at play.
Cardiologists have a negative opinion of foamy macrophages. They’re frequently observed as plaques around inflamed blood vessel sections. Foamy plaque is the most dangerous type of plaque, and it’s linked to advanced cardiovascular disease.
Beiyan Zhou, a UConn Health School of Medicine immunologist says, “We started looking at macrophages, cells that eat lipids stuck to the walls of blood vessels. They look foamy because the fat droplets are contained in the cell and look like a clump of bubbles.”
Foamy macrophages, on the other hand, maybe both more neutral and more intriguing than they’re given credit for. Zhou and colleagues from the MultiEthnic Study of Artherosclerosis (MESA) investigated the foamy cells’ lipid consumption in relation to heart attacks, arthritis, and even irritable bowel syndrome.
The researchers discovered that foamy macrophages are mostly a cleanup crew that consumes fat that has gotten stuck in the incorrect locations. Cardiovascular disease worsens if macrophages are stopped from clearing up. The lipid-eating macrophages, on the other hand, function differently in patients with diabetes, autoimmune illness, or who are taking particular immunotherapies.
“Foaming is not necessarily bad; this is the first time that we can distinguish good and bad foaming. It is the bad foaming that can cause heart attack,” Zhou says.
MESA is long-term research that analyses how cardiovascular disease develops, and Zhou and her team are working on it with UConn Health cardiologists Annabelle Rodriguez-Oquendo and Patrick Murphy, as well as immunologist Anthony Vella.
They want to figure out what triggers foamy cells to become unhealthy and disease-causing. MESA provided the scientists with a big dataset of persons who developed heart disease or did not acquire heart disease during the previous 20 years.
The scientists used MESA’s data to generate a 30-gene model from a pool of harmful foaming genes discovered by AtheroSpectrum, a programme developed by Zhou’s team. The model generated a fairly accurate score of a person’s risks of having a stroke or heart attack over the following 5 years when it was combined with clinical data on blood pressure, current medicines, and diabetes status. Their score was better than cardiologists’ current best practices for predicting adverse outcomes.
Understanding pathogenic foaming has resulted in a new approach for developing future risk assessments for heart disease patients.
Contributed by: Mithun Sukesan
To ‘science-up’ your social media feed, follow us on Facebook, Twitter or Instagram!