Researchers from the University Of Cambridge, the National Health Service and the University of Bristol in the U.K. have become the first to manufacture blood in the lab and administer it to humans. The clinical research, which has so far been already tested on two volunteers, aims to see how safe and effective this lab blood is. Researchers are hoping that this blood will be more powerful than the natural one.
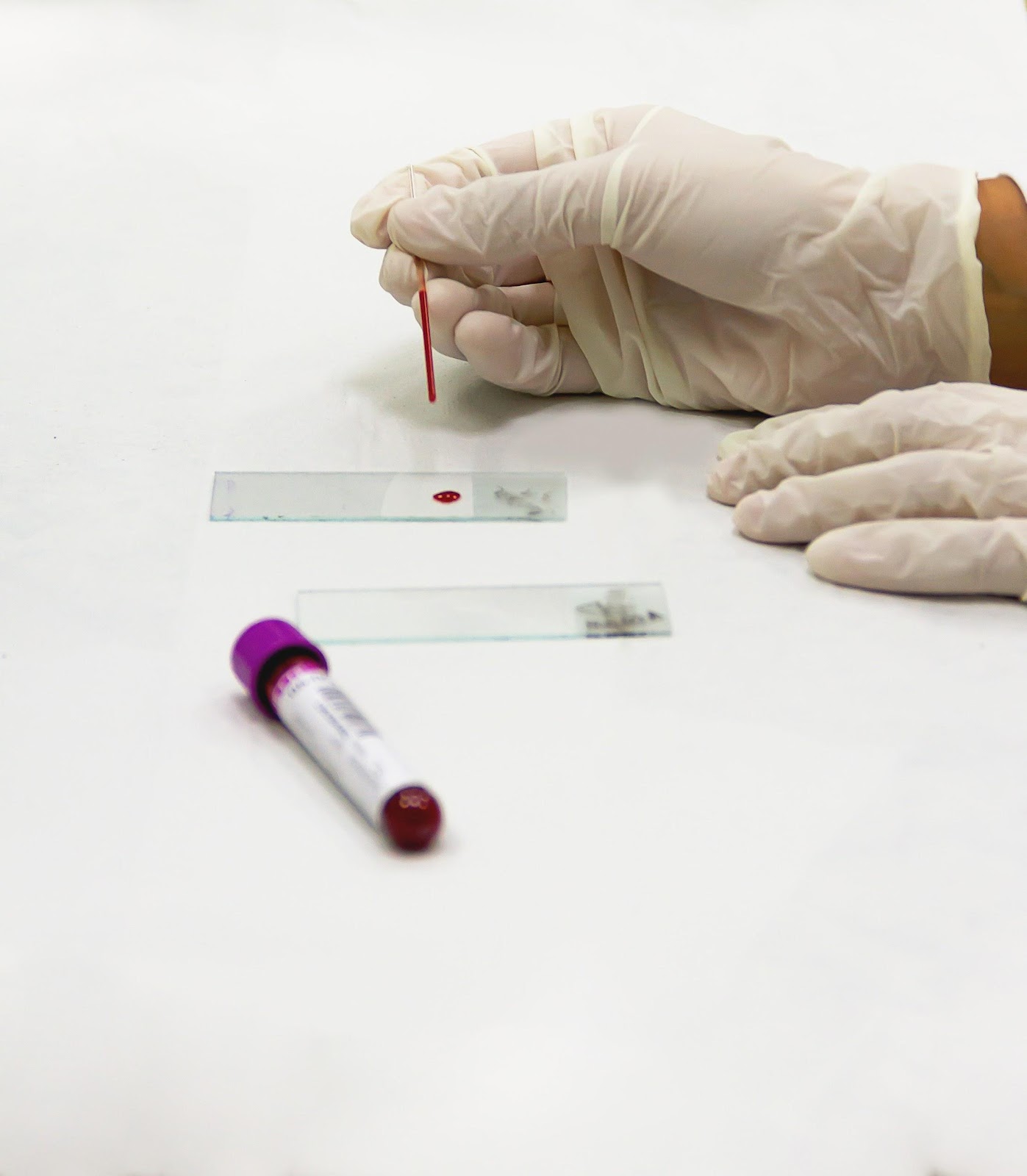
Image credit Pexels
Earlier in the 1600s, doctors in the West tried to infuse milk and wine in injured patients which didn’t prove effective. Then they tried infusing sheep’s blood which also didn’t work. In 1818 James Blundell, a British obstetrician was successful after he trialed a transfusion of a similar blood group. The main question in front of the researchers is whether their invention can be as durable as RBCs, the red blood cells which stay for almost 120 days in our body, or have any negative consequences. If researcher in the U.K. are successful in their attempts, then we could soon have artificial blood too.
How blood donations help
Blood donations have always been a lifesaver for patients. The products of blood are also used as a remedy in conditions of sickle cell anaemia which is a group of disorders that cause red blood cells to become rigid and sickle shaped. However, blood donations as a process has many drawbacks.
Firstly blood donation needs large infrastructure right from extraction to storage and transportation. It remains a challenge to find suitable blood groups for individuals which have different body types as the rare blood groups are often harder to find. With that, the blood donation infrastructure is also very costly to maintain.
How this blood is grown?
Image credit Wikimedia Commons
The method to make lab-grown blood requires the synthesis of artificial components which perform an oxygen-carrying role in blood. It focuses on the RBCs as their main role is to carry oxygen from the lungs to the rest of the body. For this the researchers started with a simple donation of blood of around 470 ml. The researchers then turned to stem cells to harness their power of flexibility and turned them into RBCs. The scientists used special magnets to do this and then transferred them into the lab environment ensuring proper arrangements so that the cells multiply themselves. This process took about three weeks and around half a million stem cells became 50 billion red blood cells. From these around 15 million were ready to be used for transplant. This might sound like a lot of cells but in healthy adults, just a microliter (0.001 ml) contain anywhere between 3.92 and 5.65 million RBCs.
The Road Ahead
Scientists have been searching for more practical options and are hopeful to make this method a success. But for now, the clinical trial is only using fewer amounts of lab-grown blood. The researchers are hoping to produce large volumes of blood for people with rare blood types. However, this remains a challenge as this system needs to speed up the technology and infrastructure at a low cost so it can be available for everyone who is in need.
If you enjoyed reading our articles, please consider supporting us by buying our geeky merchandise on Instagram
Alternatively you could Buy us a coffee or follow us on Facebook, Twitter, Pinterest or Medium!





1 comment
[…] from the patient’s bone marrow and releases them into the bloodstream. Doctors can then draw blood from the patient and harvest the stem […]