Image Credit: stock.adobe.com
Most of us depend on our bodies to fight off infections, but how often do we stop to think about just how this works? It’s commonly known that our white blood cells play a key role in eliminating intrusive bacteria or parasites and learning how to ward them off more effectively in the future. However, there are other cell types that enter the ring to fight infection. Immunologists put a lot of effort into figuring out what roles the different cells play in our immune system play and how all of these fighters strategize with each other.
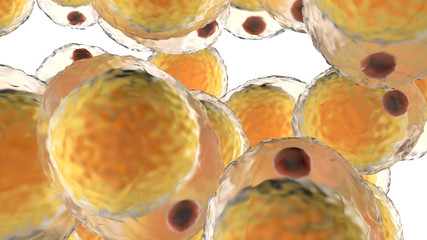
One such immunologist at the Bloomberg Kimmel Institute at Johns Hopkins University School of Medicine recently published a paper with her colleagues that explores how a special type of T lymphocytes (white blood cells that ‘remember’ infecting organisms) communicate with tissue and fat cells in response to parasitic infections. We interviewed Dr. Agnieszka Kabat (AK) to learn more.
CTS: Could you briefly summarize your results for our audience?
AK: We have focused on investigating how the body fat that surrounds the intestine is affected by infection that happens in the gut itself. We found that when the intestine becomes infected by a parasite, mesenteric fat [the body fat that surrounds the intesting] stops storing lipids, and instead starts producing fibrotic substances that make the whole tissue more rigid.
We also found that these changes are possible because a new population of immune cells – a special type of T lymphocytes called Th2 cells – appears in the fat and helps the tissue remodel. Both Th2 cells and structural cells that are normally present in the fat talk to each other to help mesenteric fat adjust to the infection.
CTS: How much of our immune response to parasitic infections takes place in connective tissue
cells?
AK: The entry points for parasitic infection (or any infection for that matter) are usually the barrier sites of our body: the tissues that are in direct contact with the external environment; for instance, skin, lungs, or intestine.
Many parasites infect either through the intestinal tract or through skin. Cells and fibrotic components that make connective tissues in our body can be found in many organs, including skin and intestine. So, in this sense, these connective tissue cells can be in proximity to infection.
As our research (and others) have shown – they really can react and respond to the infection. We are getting a better idea of how not only our immune system, but also structural cells of our body, react to infection and communicate with the immune system, to fight the infection better or to heal the tissue.
An interesting thing about responses to large parasites or toxins and venoms is that, because they need to deal with severe tissue damage (parasites are big and when they go through the tissue, they can make wounds, etc.) these cells also take part in tissue healing – they are very good at doing that.
But type 2 responses are also detrimental if they get out of hand – in these cases you get allergies, asthma or tissue fibrosis. So, in our project, by looking at parasitic infection, we are also getting some information on mechanisms that might be important in other situations, during healing or response to food allergies. for instance.
Image Credit: stock.adobe.com
CTS: What sorts of long-lasting effects does infection have on immune response cells, even after the infection has cleared?
AK: We found that long after the infection is cleared Th2 cells wait in the mesenteric fat, slowly expand there, and are ready to become activated if they sense the parasite again. In this sense, the fat that surrounds the intestine is not the same as it was before the infection – because these Th2 cells stay there.
We think that in this setting it is beneficial because the tissue “learned” how to cope with this challenge and is more ready if it comes again. But it is possible that if something about the healing process goes wrong, and Th2 cells don’t switch off their activation once the parasite is not there, you might get some more problematic changes in the tissue – for instance more fibrosis in the fat. It is therefore important to understand these processes; for the future, we are interested in studying the healing that comes after the infection in more detail.
CTS: How does the use of anthelmintics (medicines used to kill parasitic worms) change the way our cells naturally respond to infection?
AK: This depends on the type of infection, but normally it really helps the immune system. For instance, the parasite that we use in our study is very smart and has developed many ways to hide from the immune system. It can make the immune system less responsive than it should be – that is why many parasitic infections are chronic, they can last for a very long time.
By using antihelminth drugs early on, we don’t give the parasite a chance to trick the immune system so much. It also helps the immune system to develop better memory of the parasite so that the next time the animal gets infected, it can fight it off better.
CTS: What general impact do you hope your findings have on the field of immunology?
AK: Our results are just one of many which show that every tissue in our body can have unique
immune cells within it and that these immune cells communicate with structural cells in that
tissue. We are starting to appreciate that this dialog is really important, not only when dealing with an infection, but also in normal homeostatic conditions.
There is a lot of interest in understanding these tissue-resident immune cells; we are learning a lot about them now because we have better techniques to isolate and analyze them. In the case of our results, we showed that the fat surrounding our intestine can still sense infection despite not being directly affected by it, and the fat can change its structure and composition to help strengthen the intestinal wall and perhaps also help with healing it. It is actually very cool to see how plastic and versatile our adipose tissue (body fat) is.
Image Credit: stock.adobe.com
There are these chronic inflammatory diseases of the intestine called IBDs (inflammatory bowel diseases) – that are a very serious health problem worldwide. One of the features of IBD is the so-called “creeping fat”, which refers to the mesenteric fat that expands and changes in people with IBD.
We don’t fully understand why and how this works yet, but we hope that our study can help with understanding these processes by showing some of the mechanisms of how fat changes in response to intestinal infection.